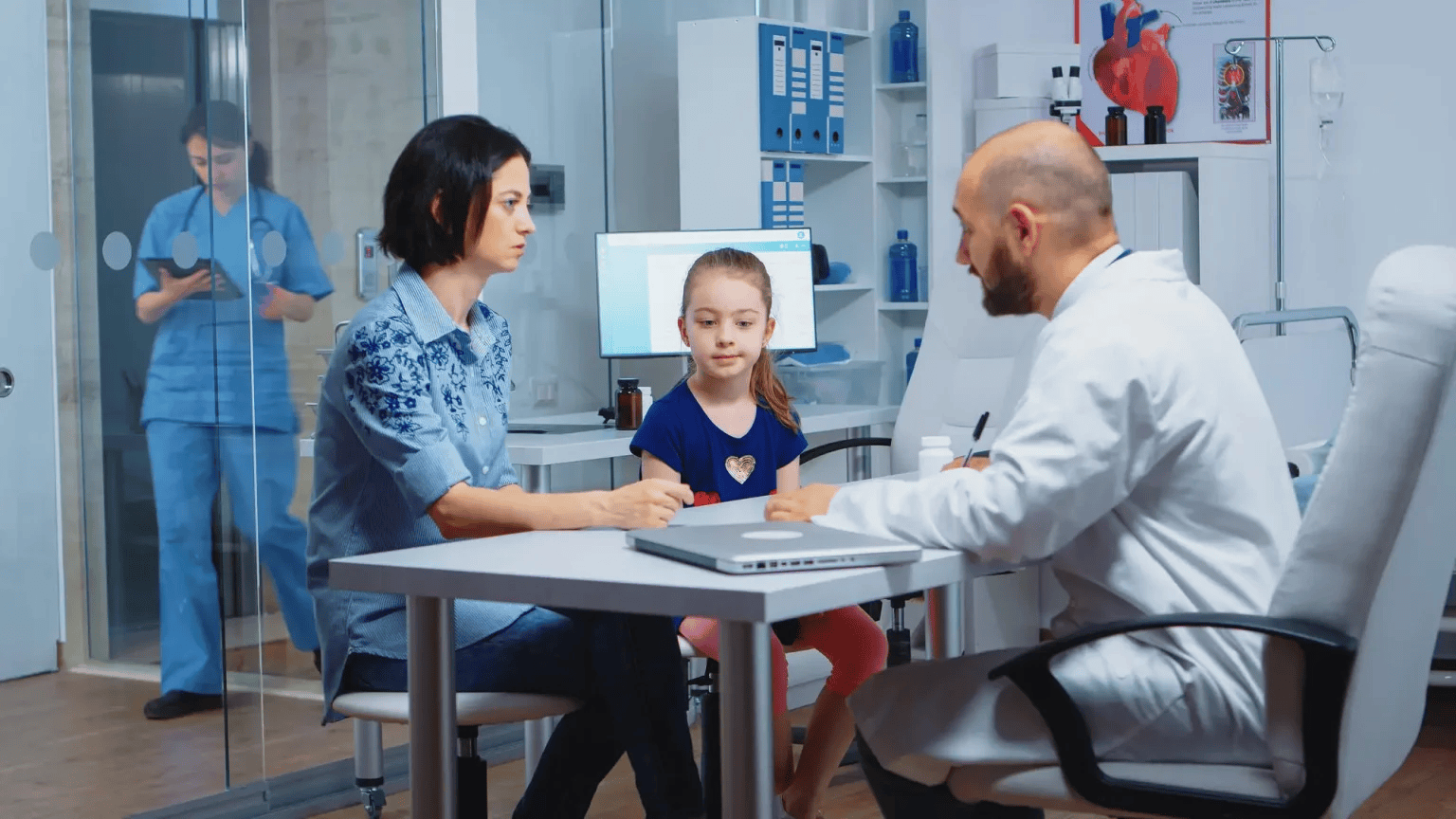
Urgent care centers in Florida operate in one of the busiest and most unpredictable healthcare environments in the country. Seasonal population shifts, high tourist traffic, and diverse insurance coverage types all contribute to complex billing challenges. This is why many facilities now turn toward an experienced emergency medical billing company in Florida that can streamline reimbursement processes, reduce denials, and help clinics maintain steady cash flow. Without expert billing support, urgent care practices often lose thousands of dollars due to improper coding, incorrect documentation, or processing delays.
Urgent care billing is far more than submitting claims—it requires precision coding, real-time verification, compliance adherence, and constant communication with insurance payers. Many in-house billing teams struggle to keep up with evolving ICD-10 updates, payer policy changes, and modifier requirements. When handled poorly, the result is claim rejections, revenue loss, and unnecessary administrative stress. Outsourcing ensures expert oversight, accurate claim submission, and faster payments for services.
Florida’s urgent care facilities deal heavily with emergency-type procedures such as suturing, X-rays, splinting, wound care, and rapid diagnostic testing. These visit types require detailed, case-specific coding to ensure accurate reimbursement. A small mistake in coding or documentation can lead to claim downcoding or complete denial. This makes professional billing support essential for urgent care centers aiming to maximize earnings while staying compliant.
As the industry continues to grow, the competition among urgent care providers also increases. Running a financially efficient clinic helps maintain competitive pricing, strong patient satisfaction, and sustainable operations. This is why outsourcing billing is becoming a standard practice—allowing medical teams to focus on treatment while experts manage revenue cycles.
Understanding the Complexity of Urgent Care Billing in Florida
Urgent care billing isn’t the same as primary care or general outpatient services. The workflow is faster, documentation must be precise, and providers often treat patients across various insurance plans—Medicare, Medicaid, commercial insurance, HMOs, and out-of-state policies. Florida’s large tourist population makes this even more complicated.
Many clinics deal with:
- High rates of insurance eligibility issues
- Incorrect coding for emergency-level procedures
- Wrong modifiers for bilateral or multiple services
- Confusion between global periods for minor procedures
- Out-of-network billing challenges
- Ever-changing payer rules
- High staff turnover
Medical staff may be excellent at patient care, but billing accuracy requires specialized experience and constant training. Outsourced billing solves these issues through systematic claim scrubbing, audit checks, and algorithm-based coding tools.
Key Challenges Florida Urgent Care Centers Face
Urgent care centers in Florida often struggle with challenges such as:
1. High Claim Denial Rates
Most claim denials occur due to:
- Missing documentation
- Wrong CPT or ICD-10 codes
- Improper modifiers
- Eligibility issues
- Timely filing mistakes
Billing experts analyze payer patterns and fix errors before claims are submitted.
2. Constantly Changing Insurance Policies
Medicare, Medicaid, and commercial insurers update coverage rules frequently. Specialized billing partners stay ahead of these updates to ensure compliance.
3. Heavy Patient Volume
Urgent care centers have high patient turnover, especially during:
- Flu seasons
- Holidays
- Tourist influx periods
This requires extremely efficient billing to avoid backlogs.
4. Difficulty Handling Out-of-Network Claims
With millions of tourists visiting Florida annually, urgent care centers deal with unfamiliar payers daily. Billing experts know exactly how to handle these claims to prevent underpayments.
How Professional Billing Enhances Revenue Growth
Revenue Cycle Management (RCM) involves more than claim submission—it includes eligibility checks, coding support, payment posting, AR follow-up, appeals, and patient billing.
By partnering with experienced professionals, urgent care clinics enjoy:
- 25–40% increase in clean claim rate
- 20–35% reduction in denials
- Faster reimbursement cycles
- Lower administrative overhead
- Improved compliance
Billing teams use advanced tools like:
- Automated claim scrubbing
- Real-time eligibility verification
- Electronic remittance tracking
- Denial trend analysis
- Compliance monitoring
The fifth paragraph here highlights the importance of advanced billing structure, which is why many urgent care practices trust full-service Medical Billing Services to improve financial stability and eliminate administrative stress.
Why Outsourcing Billing is the Best Option for Urgent Care Centers
Outsourcing urgent care billing is not just about saving time—it’s about maximizing financial outcomes.
1. Expert Coding Knowledge
Urgent care procedures often involve:
- Laceration repairs
- Fracture management
- Diagnostic imaging
- Injections and infusions
- Rapid tests
- Minor surgical procedures
Each service demands accurate coding and the correct use of modifiers such as 25, 59, RT/LT, etc.
2. Reduced In-House Workload
Front-desk teams no longer need to:
- Chase claim corrections
- Verify insurance manually
- Follow up on unpaid claims
- Manage AR aging reports
All these responsibilities shift to experienced billers.
3. Better Cash Flow Stability
Professional billing companies maintain continuous claim submission cycles, ensuring a steady flow of revenue.
4. Strict Compliance Adherence
Billing companies protect urgent care centers from:
- Medicare audits
- Medicaid errors
- Fraud allegations
- Incorrect billing practices
They ensure every claim aligns with federal and state guidelines.
Impact of Technology on Modern Urgent Care Billing
Technology has transformed medical billing, enabling faster and more accurate processes. Billing teams now use:
- AI-based coding assistance
- Real-time eligibility systems
- Automated claim correction tools
- Cloud-based billing platforms
- Data analytics dashboards
This innovation dramatically reduces errors and speeds up reimbursements.
Urgent care centers benefit from:
- Instant insurance verification
- Reduced manual entry
- Automated appointment-to-claim integration
- Faster claim submission
- Detailed financial visibility
Documentation Support for Physicians
Accurate documentation is the backbone of successful billing. Billing partners assist providers by:
- Ensuring visit notes match claim codes
- Advising on required documentation for procedures
- Reviewing medical records for completeness
- Preventing downcoding issues
- Supporting level-of-service justification
This reduces denials and improves revenue outcomes.
Special Considerations for Emergency-Level Urgent Care Services
Urgent care centers often perform emergency-level treatments. These require:
- Correct evaluation and management (E/M) coding
- Use of procedure-specific modifiers
- Accurate global period calculation
- Proper documentation of time-based services
Billing companies handle these complexities effortlessly, ensuring maximum reimbursement.
Worker’s Compensation Billing Support
Worker’s compensation claims are common in urgent care settings. They require:
- Employer information
- Injury documentation
- Special claim forms
- Adjuster communication
Billing experts manage each step to ensure timely payments.
Handling Telehealth Billing for Urgent Care
Telehealth is now a core service for urgent care centers. Billing specialists manage:
- Telehealth-specific E/M codes
- Audio vs. video visit documentation
- Payer policy variations
- Modifier requirements
This ensures clinics get paid correctly for virtual visits.
Denial Management and Appeals
Denied claims are one of the biggest sources of lost revenue. Billing companies provide:
- Root-cause analysis
- Denial categorization
- Rapid corrections
- Resubmissions
- Detailed appeals
This ensures urgent care centers recover the maximum possible revenue.
Improving Patient Billing Experience
Patients often get confused by medical bills. Billing partners improve patient satisfaction by offering:
- Clear statements
- Digital payment portals
- Easy installment plans
- Prompt customer support
This leads to higher patient trust and fewer billing disputes.
Credentialing Support for Urgent Care Facilities
Credentialing is crucial for insurance participation. Billing companies assist with:
- Enrollment in new networks
- Contract renewals
- Rate negotiations
- Follow-up with payers
This ensures clinics can serve a wider patient base.
Scalability as Your Urgent Care Center Grows
As urgent care centers expand to new locations or add new services, billing requirements increase. Outsourced billing scales effortlessly without additional staff, training, or software purchases.
Data Analytics for Stronger Financial Decisions
Billing companies offer detailed analytics, including:
- Reimbursement trends
- Payer performance insights
- Coding accuracy reports
- Denial patterns
- Financial forecasting
This helps urgent care leaders make informed decisions that strengthen profitability.
Conclusion: A Strong Billing Partner Means a Stronger Practice
Urgent care centers in Florida face unique billing challenges due to high patient volume, emergency-level treatments, and diverse insurance coverage. Partnering with a specialized billing company ensures:
- Accurate coding
- Faster reimbursements
- Fewer denials
- Lower administrative load
- Better compliance
Outsourcing allows providers to focus on what matters most—delivering high-quality care while experts optimize every part of the revenue cycle.
FAQs
1. Why should urgent care centers outsource billing?
Outsourcing reduces errors, lowers denial rates, speeds up reimbursements, and removes administrative stress from clinical teams.
2. What makes urgent care billing different from regular medical billing?
Urgent care billing involves emergency-level procedures, rapid workflows, multiple insurance types, and more complex coding requirements.
3. How does a billing company help reduce claim denials?
Billing experts use claim scrubbing tools, coding audits, and payer-specific rules to prevent errors before submission.
4. Can billing companies help with telehealth services?
Yes, they manage telehealth coding, documentation, and payer policies to ensure full reimbursement.
5. Do billing companies provide reports and financial insights?
Absolutely. Clinics receive detailed reports on revenue, denials, payer performance, and financial trends.